When considering an NT scan, it’s essential to understand the various causes and risk factors involved. Your age, family history, and environmental conditions can greatly influence the results. These elements play a key role in evaluating the risk of chromosomal abnormalities in your developing fetus. As you explore these factors, you’ll find that knowing them can shape your choices and prepare you for what lies ahead in your pregnancy journey.
Understanding Nuchal Translucency Scans
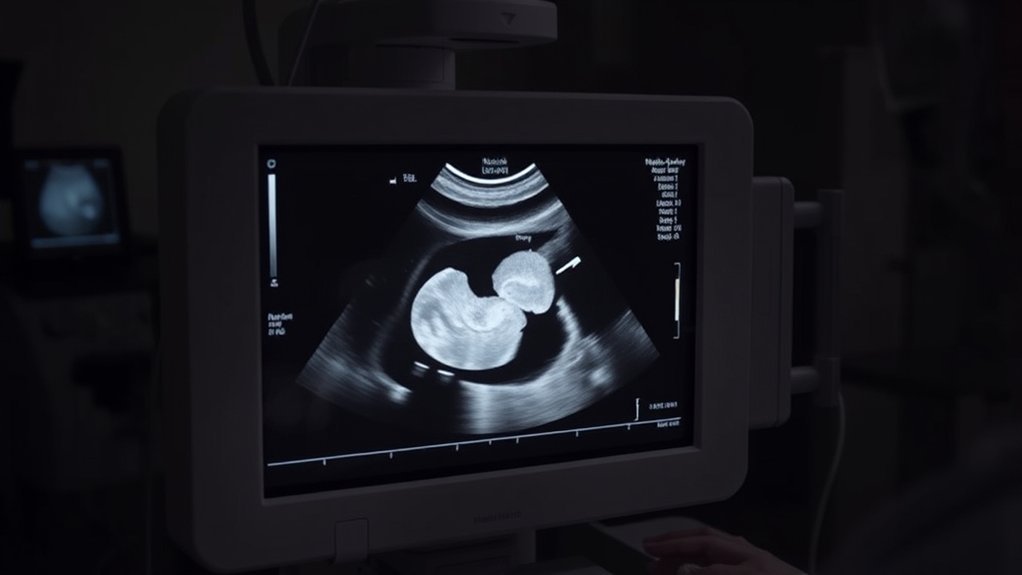
When you’re expecting, understanding a nuchal translucency (NT) scan is essential for evaluating your baby’s risk of chromosomal abnormalities.
This ultrasound test typically occurs between 11 and 14 weeks of pregnancy, measuring the fluid-filled space at the back of your baby’s neck. A thicker NT measurement can indicate a higher risk of conditions such as Down syndrome or other genetic disorders.
The NT scan is often combined with blood tests to enhance accuracy. While it’s a non-invasive procedure, remember that it doesn’t provide a definitive diagnosis; rather, it assesses risk levels.
Discuss any concerns with your healthcare provider, who can guide you on the next steps based on your results and individual circumstances.
Chromosomal Abnormalities and Their Impact

Chromosomal abnormalities, such as Down syndrome and Turner syndrome, can greatly affect fetal development.
An NT scan helps detect these disorders early in pregnancy, allowing you to make informed decisions about management options.
Understanding the implications of these findings is essential for your pregnancy planning and care.
Common Chromosomal Disorders
Approximately 1 in 150 live births is affected by a notable chromosomal disorder, highlighting the importance of understanding these abnormalities.
The most common chromosomal disorders include Down syndrome (Trisomy 21), which results from an extra chromosome 21, and Turner syndrome, where a female is partially or completely missing an X chromosome.
You might also encounter Klinefelter syndrome, characterized by an extra X chromosome in males, leading to various physical and developmental issues.
These disorders can affect physical health, cognitive abilities, and overall quality of life.
Early diagnosis and intervention can considerably improve outcomes, emphasizing the need for awareness and understanding of chromosomal disorders in prenatal care.
Detection Through NT Scan
The NT scan, or nuchal translucency scan, plays an essential role in early detection of chromosomal abnormalities during pregnancy. By measuring the thickness of the fluid at the back of the fetus’s neck, healthcare providers can assess the risk of conditions like Down syndrome.
This non-invasive procedure is typically performed between 11 and 14 weeks of gestation. An increased nuchal translucency measurement may indicate potential chromosomal issues, prompting further diagnostic testing.
It’s important to understand that while the NT scan can identify at-risk pregnancies, it doesn’t provide a definitive diagnosis. The results often lead to discussions about additional testing options, such as chorionic villus sampling or amniocentesis, to confirm any abnormalities.
Early detection is vital for informed decision-making.
Implications for Pregnancy Management
When an NT scan indicates an increased risk for chromosomal abnormalities, it can considerably influence how you manage your pregnancy.
You’ll likely undergo additional testing, such as non-invasive prenatal testing (NIPT) or amniocentesis, to confirm any abnormalities. Depending on the results, you may need to discuss potential complications and options with your healthcare provider, including the possibility of preparing for a child with special needs.
It’s vital to reflect on emotional support during this time, as the news can be overwhelming. You might also explore prenatal care adjustments or specialized consultations to guarantee best outcomes.
Ultimately, being informed and proactive about your options will empower you to navigate your pregnancy with confidence and clarity.
Maternal Age as a Risk Factor

As you consider maternal age, it’s essential to understand how it impacts chromosomal risks during pregnancy.
Advanced maternal age, typically defined as 35 years or older, is linked to an increased likelihood of chromosomal abnormalities in the fetus.
This correlation highlights the importance of discussing age-related risks with your healthcare provider.
Advanced Maternal Age
Advanced maternal age, typically defined as being 35 years or older at the time of delivery, greatly influences pregnancy outcomes.
As you age, the likelihood of experiencing complications such as gestational diabetes, hypertension, and preterm labor increases. Your chances of requiring a cesarean section also rise.
Additionally, older mothers may face a higher risk of low birth weight or fetal growth restriction. It’s essential to stay informed about these potential challenges as you plan your pregnancy.
Regular prenatal care becomes even more important, allowing you to monitor your health and that of your baby closely.
Age-Related Chromosomal Risks
Maternal age greatly impacts chromosomal health, increasing the likelihood of genetic abnormalities. As you age, particularly past 35, the risk of conditions like Down syndrome rises considerably. This is primarily due to the aging of oocytes, which can lead to errors during cell division.
These chromosomal anomalies often result from improper segregation of chromosomes, a process that becomes less efficient with age. Additionally, older maternal age is associated with higher rates of miscarriage and stillbirth, further complicating pregnancy outcomes.
It’s essential to understand these risks when planning for pregnancy, as they can influence your prenatal screening options and overall reproductive health strategy. Consulting with a healthcare provider can help you navigate these considerations effectively.
Genetic History and Family Background
Understanding your genetic history and family background can greatly influence the assessment of risks associated with NT scans. If you have a family history of chromosomal abnormalities, such as Down syndrome or other genetic disorders, it’s vital to share this information with your healthcare provider. They’ll consider these factors when interpreting NT scan results.
Additionally, certain inherited conditions may elevate risks for your fetus, making it essential to discuss any relevant genetic testing done in your family. Knowing your ancestry can also reveal potential hereditary issues, allowing for more informed decision-making throughout your pregnancy.
Environmental Influences on Fetal Development
While many factors contribute to fetal development, environmental influences play an essential role in shaping health outcomes. Various external elements can affect how a fetus grows and develops, potentially leading to complications or health issues.
Awareness of these influences is important for expectant parents.
- Pollution: Exposure to air and water pollutants can lead to developmental problems.
- Nutrition: A balanced diet provides essential nutrients; deficiencies can hinder growth.
- Toxins: Chemicals in household products and pesticides may adversely affect fetal health.
- Stress: High levels of maternal stress can impact fetal development and birth outcomes.
Importance of Follow-Up Testing and Counseling
Environmental factors can greatly impact fetal health, making follow-up testing and counseling essential for expectant parents. After an NT scan, it’s vital to understand your results and any potential implications. Follow-up testing helps clarify risks and guides informed decisions. Counseling offers emotional support and practical advice, addressing concerns about possible outcomes.
| Testing Type | Purpose | Timing |
|---|---|---|
| Blood Tests | Assess chromosomal issues | 10-14 weeks gestation |
| Ultrasound | Evaluate fetal anatomy | 18-20 weeks gestation |
| Genetic Counseling | Discuss genetic risks | Anytime during pregnancy |
| Non-invasive Testing | Identify genetic disorders | 10-20 weeks gestation |
| Amniocentesis | Confirm genetic conditions | 15-20 weeks gestation |
Engaging with healthcare providers guarantees you’re well-informed and supported throughout your pregnancy journey.
Frequently Asked Questions
How Is Nuchal Translucency Measured During the Scan?
During the scan, you lie down while a sonographer uses an ultrasound probe on your abdomen. They measure the fluid at the back of your baby’s neck, determining nuchal translucency thickness for assessment purposes.
Are There Any Risks Associated With the NT Scan Itself?
While the NT scan’s risks are minimal, you should know that there’s a slight chance of discomfort or anxiety. Most importantly, it’s non-invasive and doesn’t involve radiation, making it generally safe for you and your baby.
What Should I Do if My NT Scan Result Is Abnormal?
If your NT scan result is abnormal, consult your healthcare provider promptly. They’ll discuss further testing options, potential implications, and any necessary follow-up procedures to guarantee you understand your situation and available choices.
Can the NT Scan Be Performed at Any Stage of Pregnancy?
You can typically have the NT scan performed between 11 and 14 weeks of pregnancy. It’s essential to schedule it during this window for accurate results and early risk assessment regarding chromosomal abnormalities.
How Accurate Is the NT Scan in Detecting Abnormalities?
The NT scan’s accuracy in detecting abnormalities hovers around 80-90%. It means if your results show potential issues, you’ll want follow-up testing, as early detection can greatly impact your pregnancy journey and options.
Conclusion
In summary, understanding the Nuchal Translucency scan‘s significance helps you assess risks, recognize factors, and make informed choices. By acknowledging maternal age, genetic history, and environmental influences, you empower yourself to navigate potential challenges. Prioritizing follow-up testing and counseling not only enhances your awareness but also strengthens your support network. Ultimately, being proactive guarantees you’re prepared for the journey ahead, safeguarding both your health and your baby’s well-being during this critical time in pregnancy.
