Steering the waters of pregnancy can feel like walking a tightrope, especially when it comes to uterine rupture risk. Understanding the factors that contribute to this complication is essential for your safety and that of your baby. By recognizing the symptoms and knowing your options, you can take proactive steps. But what should you really be aware of during this critical time? Let’s explore the essential components of managing this risk effectively.
Understanding Uterine Rupture
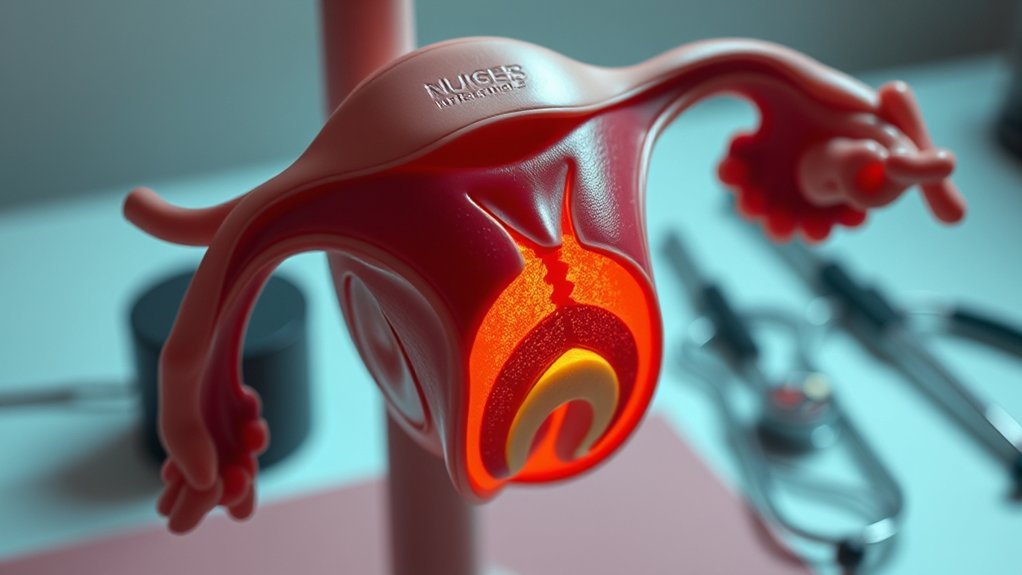
Uterine rupture occurs when the wall of the uterus tears during pregnancy or childbirth, and while it’s rare, understanding its implications is vital for expectant mothers and healthcare providers.
This condition can lead to severe complications for both the mother and the baby. Symptoms may include sudden abdominal pain, vaginal bleeding, and changes in fetal heart rate, which require immediate medical attention.
Diagnosis typically involves imaging studies or direct observation during labor. Treatment usually necessitates emergency surgery, often a cesarean section, to prevent further complications.
Your awareness of uterine rupture can facilitate timely medical interventions, ultimately protecting both you and your baby. Recognizing the signs and understanding the urgency of this condition is essential for ensuring the best outcomes.
Common Risk Factors
When considering the risk of uterine rupture, it’s essential to be aware of common risk factors.
A history of previous uterine surgery and multiple pregnancies can greatly increase your risk.
Understanding these factors can help you and your healthcare provider make informed decisions about your pregnancy management.
Previous Uterine Surgery
Having a history of previous uterine surgery can greatly increase the risk of uterine rupture during pregnancy and labor.
Surgeries such as cesarean sections, myomectomies, or any procedure involving uterine incisions can compromise the structural integrity of your uterus. Scar tissue may form, leading to weaknesses that can result in rupture when under the stress of contractions.
If you’ve had a cesarean delivery, the type of incision—classical versus low transverse—can also influence risk.
It’s essential to inform your healthcare provider about any past surgeries, as they may recommend closer monitoring or alternative delivery methods to mitigate risks.
Understanding your surgical history helps guide safe practices during your pregnancy journey. Always prioritize open communication with your healthcare team.
Multiple Pregnancies History
A history of multiple pregnancies can elevate your risk of uterine rupture, particularly if you’ve experienced several births in a relatively short timeframe. Each pregnancy places stress on the uterine wall, and this cumulative effect can weaken the tissue, increasing the likelihood of rupture during subsequent deliveries.
Additionally, the type of delivery—whether vaginal or cesarean—can further influence this risk. If you’ve had multiple cesarean sections, the presence of scar tissue may complicate future pregnancies.
It’s essential to discuss your delivery history with your healthcare provider, as they can assess your individual risk factors and recommend appropriate monitoring and management strategies. Understanding these risks can help you make informed decisions for future pregnancies.
Identifying Symptoms
Recognizing the symptoms of uterine rupture is essential for timely intervention.
You should be alert to common warning signs, including significant pain and discomfort, as well as emergency symptoms.
Understanding these indicators can help guarantee you seek medical attention when necessary.
Common Warning Signs
How can you tell if you’re experiencing the early signs of uterine rupture? Recognizing these warning signs is vital for your safety and the well-being of your baby.
Pay attention to the following symptoms:
- Sudden onset of vaginal bleeding
- Unusual abdominal tenderness or tightness
- Changes in fetal movement patterns
- Increased heart rate or palpitations
If you notice any of these signs, it’s essential to seek immediate medical attention.
Early intervention can greatly reduce risks associated with uterine rupture. Always communicate any concerns with your healthcare provider, as they can guide you through appropriate actions and monitoring.
Your awareness and vigilance are key to ensuring a safer pregnancy experience.
Pain and Discomfort
While experiencing discomfort during pregnancy can be common, distinguishing between typical aches and potential signs of uterine rupture is vital. You may notice sharp, sudden pain in your abdomen, which could indicate a serious issue.
Pay attention if this pain is accompanied by unusual pressure or a feeling of fullness. Additionally, persistent back pain, especially if it feels different from your usual discomfort, warrants careful observation.
It’s significant to recognize any changes in fetal movement; decreased movement might signal complications. Trust your instincts; if something feels off, it’s imperative to consult your healthcare provider.
Recognizing these symptoms early can make a substantial difference in ensuring your safety and that of your baby. Stay vigilant and proactive.
Emergency Symptoms to Watch
If you experience sudden and severe abdominal pain, it’s essential to assess the situation immediately, as this could indicate a uterine rupture.
This condition can escalate quickly, so recognizing additional emergency symptoms is critical.
Look out for the following signs:
- Heavy vaginal bleeding: A significant amount of blood loss can signal a serious problem.
- Dizziness or fainting: These symptoms may indicate shock from blood loss.
- Rapid heart rate: An increased pulse can be a response to internal distress.
- Loss of fetal movement: If you notice a sudden decrease in fetal activity, seek medical attention promptly.
Addressing these symptoms right away can be imperative for both your safety and that of your baby.
The Role of Previous Cesarean Deliveries
Previous cesarean deliveries considerably influence the risk of uterine rupture in subsequent pregnancies.
Previous cesarean deliveries significantly affect the risk of uterine rupture in future pregnancies.
When you’ve had a cesarean, the uterine scar from the surgery can weaken, making rupture more likely during labor. The risk increases with the number of previous cesarean sections; each additional surgery can compound the potential for complications.
Research indicates that women with one prior cesarean have a lower risk compared to those with two or more.
It’s essential to discuss your delivery options with your healthcare provider, as they can help assess your individual risk factors. They may recommend a trial of labor after cesarean (TOLAC) or a repeat cesarean, depending on your specific medical history and circumstances.
Understanding these risks empowers you to make informed decisions.
Impact of Labor Induction Methods
Labor induction methods can significantly affect the risk of uterine rupture, particularly in women with a history of cesarean deliveries. Understanding these methods is essential for managing potential complications during labor.
Consider the following factors:
- Prostaglandins: These can soften the cervix but may increase contraction intensity, raising rupture risks.
- Oxytocin: Commonly used for induction, high doses can lead to overstimulation and increased uterine pressure.
- Mechanical methods: These may provide a gentler approach, but risks still exist depending on individual circumstances.
- Timing and monitoring: Close observation during induction is important to identify early signs of complications.
Monitoring During Pregnancy
Monitoring during pregnancy is essential for ensuring both maternal and fetal well-being, especially for women at higher risk of complications. Regular check-ups help identify any potential issues early. Your healthcare provider may recommend specific tests or monitoring strategies based on your unique situation. Vaccination can further enhance overall maternal and infant health by protecting against infections that can affect pregnancy outcomes.
| Monitoring Method | Purpose | Frequency |
|---|---|---|
| Ultrasound | Assess fetal growth and anatomy | Every trimester |
| Fetal Heart Rate Monitoring | Evaluate fetal well-being | As needed, often in third trimester |
| Maternal Blood Tests | Monitor health markers | First and second trimester, as needed |
Emergency Response Procedures
In the event of a suspected uterine rupture, immediate action is crucial for the safety of both mother and baby.
You should follow these emergency response procedures promptly:
- Call for Help: Notify your healthcare provider or emergency services immediately.
- Monitor Critical Signs: Keep track of the mother’s pulse, blood pressure, and fetal heart rate if possible.
- Position the Mother: Lay her on her left side to improve blood flow and relieve pressure on major blood vessels.
- Prepare for Transport: Confirm that any necessary medical equipment is ready for quick transfer to a hospital.
Acting swiftly can greatly impact outcomes.
Swift action can significantly influence the health and safety of both mother and baby.
Always prioritize clear communication with medical professionals to guarantee the best care for both mother and baby.
Preventive Measures for Expecting Mothers
While every pregnancy carries some risk, expecting mothers can take proactive steps to minimize the likelihood of uterine rupture.
First, consider your obstetric history; if you’ve had previous cesarean deliveries, discuss your delivery options with your healthcare provider early on.
Maintain a healthy lifestyle by eating a balanced diet and engaging in appropriate exercise, as this supports overall well-being.
Regular prenatal care is essential for monitoring your pregnancy and identifying any potential complications.
Avoid high-stress situations and follow recommended guidelines for labor and delivery.
Stay informed about the signs of complications, and prioritize rest, as fatigue can increase risks. Additionally, advanced labor, delivery, and postpartum care can significantly improve outcomes for mothers and their babies.
Importance of Communication With Healthcare Providers
Maintaining open lines of communication with your healthcare providers greatly enhances your ability to navigate the complexities of pregnancy and childbirth.
You should feel empowered to discuss any concerns or symptoms that arise. Effective communication helps in identifying risks, including uterine rupture, and guarantees timely interventions.
- Share your complete medical history.
- Report any unusual symptoms immediately.
- Ask questions about your treatment options.
- Discuss your birth plan and any preferences.
Additionally, consider participating in doula-led prenatal education classes to better understand your pregnancy journey and enhance your ability to communicate your needs.
Frequently Asked Questions
Can Uterine Rupture Occur During a Vaginal Birth After Cesarean?
Yes, uterine rupture can occur during a vaginal birth after cesarean. The risk is generally low, but factors like the type of incision and the number of previous cesareans can increase it. Always consult your healthcare provider.
What Are the Long-Term Effects of a Uterine Rupture on Future Pregnancies?
A uterine rupture can lead to complications in future pregnancies, including increased risks of placental issues, preterm birth, and the need for surgical interventions. Monitoring and careful planning are essential for ensuring safer outcomes in subsequent pregnancies.
How Is Uterine Rupture Diagnosed in a Non-Emergency Setting?
In a non-emergency setting, you diagnose uterine rupture through a patient’s medical history, physical examination, and imaging studies like ultrasound or MRI, evaluating for abnormal findings such as fluid collections or fetal heart rate abnormalities.
Are There Specific Lifestyle Changes to Reduce Uterine Rupture Risk?
To reduce uterine rupture risk, you should maintain a healthy weight, manage chronic conditions, avoid smoking, and follow a balanced diet. Regular prenatal care and open communication with your healthcare provider are also essential.
What Are the Chances of Uterine Rupture in a First-Time Pregnancy?
In a first-time pregnancy, the chances of uterine rupture are relatively low, typically ranging between 0.5% to 1%. However, factors like previous surgeries or complications can increase this risk, so monitor your health closely.
Conclusion
In managing uterine rupture risk, staying proactive is key. By understanding your personal risk factors and maintaining open lines of communication with your healthcare team, you can better navigate the challenges of pregnancy and labor. Remember, an ounce of prevention is worth a pound of cure; regular monitoring and timely intervention can make all the difference. Trust your instincts and prioritize your health for a safer delivery experience.