Prolapse may seem like a rare issue, but it affects many individuals as they age or after childbirth. Understanding the various types, causes, and symptoms can help you recognize if it’s an issue for you. This guide will walk you through essential aspects of prolapse, including treatment options and lifestyle changes that can make a difference. By staying informed, you can take proactive steps toward better pelvic health.
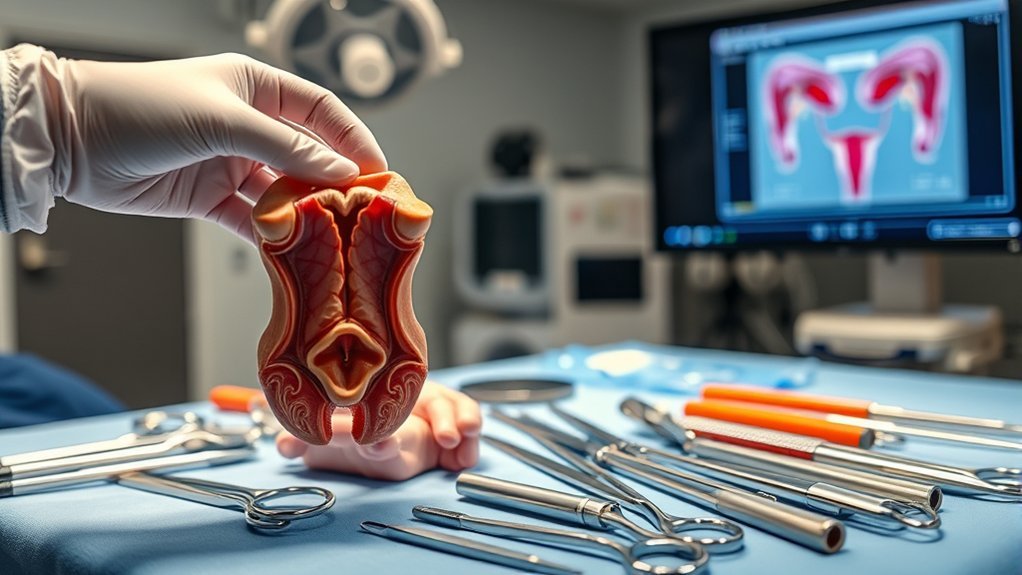
What Is Prolapse?
Prolapse refers to the condition where an organ slips out of its normal position, often due to weakened support structures. You might experience prolapse in various organs, including the bladder, uterus, or rectum.
This condition can result from factors like aging, childbirth, or chronic coughing, which all contribute to the weakening of supportive tissues. When an organ prolapses, it can lead to symptoms such as discomfort, pressure, or incontinence.
It’s essential to recognize these signs early, as they can affect your quality of life. Although prolapse can be distressing, understanding the condition helps you seek appropriate medical advice.
Early intervention can greatly improve your situation, so don’t hesitate to consult a healthcare professional if you suspect you’re experiencing prolapse.
Types of Prolapse
There are several types of prolapse, each affecting different organs in the body. The most common types include pelvic organ prolapse, which can involve the bladder (cystocele), uterus (uterine prolapse), or rectum (rectocele).
In a cystocele, the bladder pushes against the front wall of the vagina, while a rectocele occurs when the rectum bulges into the back wall. Uterine prolapse happens when the uterus descends into the vaginal canal.
You might also encounter vaginal vault prolapse, which occurs after a hysterectomy. Each type can cause varying symptoms, such as discomfort, pressure, or urinary issues. Identifying the specific type helps guide effective treatment options tailored to your needs.
Causes of Prolapse
Prolapse can occur due to various anatomical weaknesses in the pelvic support structures.
Your lifestyle and overall health also play significant roles in increasing the risk of this condition.
Understanding these factors can help you take proactive steps to manage or prevent prolapse.
Anatomical Weakness Factors
When considering the causes of prolapse, anatomical weakness factors play an essential role in its development. These weaknesses can stem from various sources, affecting the pelvic floor’s ability to support surrounding organs.
Understanding these factors helps you grasp why prolapse may occur.
- Genetic predisposition: Some individuals inherit weaker connective tissues.
- Childbirth trauma: Vaginal deliveries, especially multiple or traumatic ones, can weaken pelvic support.
- Aging: As you age, hormonal changes and natural wear and tear can diminish tissue strength.
Recognizing these anatomical weaknesses can aid in prevention and management strategies.
Lifestyle and Health Impact
Anatomical weaknesses aren’t the only contributors to prolapse; lifestyle choices and overall health greatly influence its risk. Engaging in high-impact activities, such as heavy lifting or intense exercise, can increase pressure on pelvic organs.
Additionally, obesity strains these structures, making prolapse more likely. Smoking can impair tissue health, while chronic coughs from smoking further exacerbate this risk. A diet low in fiber may lead to constipation, which can create additional strain during bowel movements.
Hormonal changes, particularly during menopause, can weaken pelvic support. It’s essential to maintain a healthy weight, stay active with low-impact exercises, and adopt a balanced diet.
These proactive steps can greatly reduce your risk of developing prolapse and enhance your overall well-being.
Common Symptoms of Prolapse
If you experience a feeling of pressure or heaviness in your pelvic region, it might signal a prolapse.
Other common symptoms can include:
- A noticeable bulge or protrusion in your vagina
- Discomfort or pain during sexual intercourse
- Urinary issues, such as incontinence or frequent urination
These symptoms can vary in intensity and may worsen with activities like lifting or prolonged standing.
It’s crucial to pay attention to these signs, as they can affect your daily life and overall well-being.
If you notice any of these symptoms, consider consulting a healthcare professional for a proper evaluation.
Early recognition and management of prolapse can help improve your quality of life considerably.
Risk Factors for Prolapse
As you age, hormonal changes can greatly impact your risk of developing prolapse.
Lifestyle choices and genetic factors also play essential roles in this condition.
Understanding these risk factors can help you take proactive steps to maintain your pelvic health.
Age and Hormonal Changes
While aging is a natural part of life, it greatly influences the risk of developing prolapse, particularly due to hormonal changes. As you age, your body experiences a decline in estrogen levels, which can weaken pelvic floor muscles and connective tissues. This weakening can lead to an increased risk of prolapse.
Consider these factors:
- Menopause: The drop in estrogen during menopause can accelerate tissue deterioration.
- Childbirth History: Multiple pregnancies can strain pelvic support structures.
- Genetic Predisposition: A family history of prolapse can heighten your risk.
Understanding these age-related and hormonal influences is essential for recognizing your risk and taking proactive steps to maintain pelvic health.
Stay informed and consult with your healthcare provider if you have concerns.
Lifestyle and Genetic Factors
Lifestyle choices and genetic factors play a significant role in your risk of developing prolapse. Factors like obesity, smoking, and lack of exercise can weaken pelvic support structures. Additionally, a family history of prolapse may increase your risk due to inherited connective tissue weaknesses.
| Lifestyle Factors | Genetic Factors | Impact on Prolapse |
|---|---|---|
| Obesity | Family History | Increased risk |
| Smoking | Genetic Disorders | Weakened tissues |
| Sedentary Lifestyle | Age-related Changes | Compromised support |
Understanding these risk factors can help you make informed choices. By addressing lifestyle habits and being aware of your genetic predispositions, you can potentially reduce your risk of developing prolapse.
Diagnosing Prolapse
How can you recognize if you have a prolapse? Identifying the signs and symptoms early can help you address the issue effectively.
Common indicators include:
- A feeling of pressure or heaviness in the pelvic area
- Visible bulging or protrusion from the vagina
- Discomfort or pain during intercourse
If you notice any of these symptoms, it’s essential to consult a healthcare professional for a thorough evaluation.
They’ll typically perform a pelvic exam and may ask about your medical history and any accompanying symptoms.
Early diagnosis can lead to better outcomes, so don’t hesitate to seek help. Understanding your body and its signals is vital in identifying a prolapse and taking the next appropriate steps.
Treatment Options for Prolapse
When you’re faced with a prolapse, understanding your treatment options is essential for managing symptoms and improving your quality of life.
You can start with conservative approaches, like pelvic floor exercises, which strengthen the muscles supporting your pelvic organs. Another option is the use of a pessary, a device inserted into the vagina to support the prolapsed organ.
Conservative treatments like pelvic floor exercises and pessaries can effectively support pelvic organ health.
If these methods don’t provide relief, surgical intervention may be necessary. Surgical options vary based on the type of prolapse and may include repairing the pelvic floor or removing excess tissue.
Discussing these options with your healthcare provider will help you determine the best approach tailored to your needs. Remember, early intervention often leads to better outcomes.
Lifestyle Changes to Manage Prolapse
Managing a prolapse often includes making specific lifestyle changes that can greatly improve your symptoms. By adopting healthier habits, you can enhance your comfort and overall well-being.
Here are key changes to reflect upon:
- Maintain a healthy weight: Reducing excess weight can alleviate pressure on pelvic organs.
- Engage in pelvic floor exercises: Strengthening your pelvic muscles helps support your organs effectively.
- Avoid heavy lifting: Minimize activities that strain your pelvic area to prevent worsening symptoms.
Incorporating these adjustments into your daily routine can lead to significant improvements.
It’s vital to listen to your body and consult with healthcare professionals for personalized advice.
Emotional and Psychological Impact of Prolapse
Prolapse can substantially affect your emotional and psychological well-being, often leading to feelings of anxiety, embarrassment, or depression.
You might find yourself worrying about daily activities, intimacy, or even how others perceive you. These concerns can create a cycle of stress that impacts your relationships and overall quality of life.
It’s common to feel isolated, as the topic of prolapse is often stigmatized, making it hard to talk about. You may also experience frustration as you navigate your symptoms and their effects on your daily routine.
Acknowledging these feelings is vital. Support groups or counseling can help you cope, allowing you to share experiences and gain strategies for managing this complex emotional landscape.
When to Seek Medical Advice
If you notice symptoms like persistent discomfort, pelvic pressure, or changes in bladder or bowel habits, it’s important to consult a healthcare professional.
If you experience discomfort, pelvic pressure, or changes in bladder habits, consult a healthcare professional.
Prolapse can vary in severity, and early intervention can help manage symptoms effectively. Don’t hesitate to seek advice if you experience:
- A noticeable bulge in the vaginal area
- Pain during intercourse
- Frequent urinary infections or incontinence
These signs could indicate a prolapse needing medical evaluation. Your healthcare provider can offer guidance on treatment options, lifestyle changes, or pelvic floor therapy.
Frequently Asked Questions
Can Prolapse Affect Sexual Function or Pleasure?
Yes, prolapse can affect sexual function and pleasure. You might experience discomfort or changes in sensation, which can impact intimacy. It’s crucial to discuss any concerns with a healthcare professional for personalized guidance and support.
Is Prolapse Hereditary or Genetic?
Prolapse isn’t directly hereditary, but genetic factors can influence connective tissue strength. If your family has a history of prolapse or related issues, you might be more susceptible. It’s wise to discuss concerns with your doctor.
How Does Prolapse Impact Pregnancy and Childbirth?
Prolapse can complicate pregnancy and childbirth, potentially causing discomfort or increased risk during delivery. You might experience changes in pelvic support, which could affect labor progression and the need for interventions, like cesarean sections.
What Are the Long-Term Effects of Untreated Prolapse?
Untreated prolapse can lead to chronic pain, urinary incontinence, and bowel dysfunction. You might also experience sexual dysfunction and increased risk of infections, impacting your overall quality of life and potentially worsening the condition over time.
Are There Specific Exercises to Avoid With Prolapse?
Yes, you should avoid high-impact exercises like running, jumping, or heavy lifting, as they can worsen prolapse symptoms. Focus instead on low-impact activities, core strengthening, and pelvic floor exercises to maintain support and improve your condition.
Conclusion
In summary, understanding prolapse is essential for maintaining your pelvic health. With early intervention and the right treatment options, you can reclaim control over your body and enhance your quality of life. Don’t let prolapse feel like an insurmountable mountain; taking proactive steps can bring you back to feeling like your vibrant self. Remember, open conversations with your healthcare provider are key to effective management—don’t hesitate to seek help if you notice any symptoms.