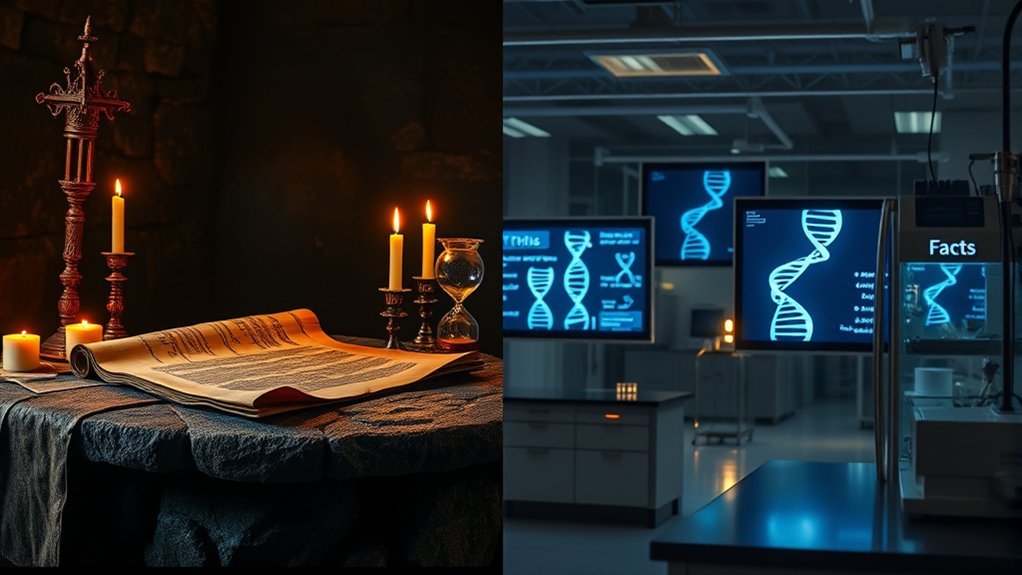
Like the myths surrounding ancient heroes, misconceptions about NIPT can cloud your understanding of this important prenatal test. Many believe it’s solely for high-risk pregnancies, but that’s just one of several misunderstandings. In reality, NIPT offers valuable insights for all expecting parents. So, what are the true benefits and limitations of this screening method? Let’s clarify the facts that can guide your prenatal decisions.
Understanding NIPT: What It Is and How It Works
When you’re expecting a baby, understanding the options for prenatal testing is essential, and that’s where Non-Invasive Prenatal Testing (NIPT) comes in.
NIPT analyzes small fragments of fetal DNA circulating in your bloodstream, providing information about potential genetic conditions. Typically performed at or after the 10th week of pregnancy, it can assess the risk of conditions like Down syndrome and other chromosomal abnormalities. [ACOG infographic]
NIPT analyzes fetal DNA in your bloodstream to assess risks for genetic conditions like Down syndrome, as early as 10 weeks.
The test involves a simple blood draw, making it safe for both you and your baby. NIPT shows high sensitivity for certain conditions (for example, ~99% for trisomy 21 in meta-analyses), and results often arrive within about 3–7 business days (timing varies by laboratory). [evidence] [turnaround]
This method empowers you with critical information while minimizing risks associated with more invasive procedures.
Myth 1: NIPT Is Only for High-Risk Pregnancies
Many people believe that Non-Invasive Prenatal Testing (NIPT) is only necessary for women considered high-risk due to age or previous pregnancy complications. However, that’s a misconception.
NIPT is available to all pregnant people, regardless of their risk status. This testing can provide valuable information about chromosomal conditions like Down syndrome and can be beneficial for anyone seeking early insight into their baby’s health.
The American College of Obstetricians and Gynecologists (ACOG) recommends that prenatal genetic screening options (including cell-free DNA/NIPT) and diagnostic testing be offered to all pregnant patients, and notes that cell-free DNA is the most sensitive and specific screening test for common aneuploidies.
Ultimately, NIPT serves as a useful tool for all expecting parents.
Myth 2: NIPT Guarantees a Healthy Baby
While NIPT provides valuable insights into potential chromosomal abnormalities, it doesn’t guarantee a healthy baby. NIPT primarily screens for specific genetic conditions, but it can’t detect all possible health issues. Understanding this limitation is vital for expecting parents.
| Condition Detected | NIPT Result | Implication |
|---|---|---|
| Down Syndrome (Trisomy 21) | Positive/High Risk | Further diagnostic testing needed (e.g., CVS or amniocentesis) |
| Trisomy 18 (Edwards syndrome) | Negative/Low Risk | Does not rule out other conditions |
| Overall screen | Negative/Low Risk | Doesn’t assure no other health issues |
It’s important to discuss your NIPT results with a healthcare provider. They can help interpret what these results mean for you and your baby, guiding you through the next steps for thorough prenatal care. In the U.S., the FDA has cautioned that NIPT is a screening test and false positives/negatives can occur; positive screens should be confirmed with diagnostic testing.
Myth 3: NIPT Is Invasive and Risky
NIPT, or non-invasive prenatal testing, is often misunderstood as an invasive procedure. In reality, it’s a simple blood test that analyzes fetal DNA circulating in your bloodstream.
Unlike invasive tests, such as amniocentesis or chorionic villus sampling, NIPT poses no risk of miscarriage or complications associated with needle procedures. This testing can be performed as early as 10 weeks into your pregnancy and requires only a small sample of your blood. [source]
Studies show that NIPT has a high accuracy for detecting certain chromosomal conditions, making it a safe and reliable option for expectant parents. [overview]
Myth 4: NIPT Can Replace All Prenatal Testing
Although NIPT offers valuable insights into fetal health, it doesn’t replace all prenatal testing. NIPT primarily screens for certain chromosomal conditions, such as Down syndrome, using a simple blood sample. However, it doesn’t provide information about other potential issues, like structural abnormalities or conditions not covered by the test.
For this reason, traditional ultrasounds and other diagnostic tests remain vital. These tests can assess fetal development and detect physical anomalies. ACOG recommends that all patients be offered a second-trimester ultrasound for structural defects, ideally at 18–22 weeks. [guidance]
In addition, if your NIPT results indicate a potential issue, you may need further testing, such as amniocentesis or chorionic villus sampling (CVS), for confirmation. Relying solely on NIPT could leave you without significant information about your pregnancy, so it’s best to use it as part of a thorough prenatal care plan.
Frequently Asked Questions
How Accurate Is NIPT Compared to Other Prenatal Tests?
NIPT’s sensitivity is higher than many traditional prenatal tests—for example, about 99% sensitivity for Down syndrome (T21) has been reported in meta-analyses—though positive predictive value depends on your baseline risk. Discuss results with your healthcare provider for interpretation and next steps. [evidence] [overview]
When Is the Best Time to Have NIPT Done?
Timing’s everything! You can have NIPT any time from 10 weeks onward (many opt for 10–13 weeks). This provides accurate results early and allows informed decisions and any necessary follow-up testing. [source]
Does NIPT Detect All Genetic Disorders?
NIPT doesn’t detect all genetic disorders; it primarily screens for specific chromosomal conditions (commonly trisomies 21, 18, and 13; some panels include sex chromosome differences). Talk with your healthcare provider about what NIPT can and can’t identify and whether additional screening or diagnostic tests are appropriate. [overview]
Can NIPT Determine the Baby’s Gender?
Yes—NIPT can report fetal sex (chromosomal sex) as early as 10 weeks by detecting the presence or absence of Y-chromosome sequences in maternal blood. Note that “sex” refers to chromosomes; “gender” is a separate personal identity. [how it’s inferred]
What Happens if NIPT Results Are Abnormal?
If your NIPT results are abnormal, you’ll typically undergo further testing, like amniocentesis or CVS, to confirm findings. Genetic counseling and a comprehensive ultrasound are recommended to guide personalized next steps. [ACOG] [ACOG/FDA statement]
Conclusion
In summary, understanding NIPT is essential for all expecting parents—it’s not just for the high-risk elite! While it offers remarkable insights, it doesn’t guarantee a perfect baby or replace all testing. Think of it as a powerful tool, not a magic wand. By clearing up these myths, you empower yourself to make informed choices in your prenatal journey. Embrace the knowledge, and remember: every pregnancy is unique, just like the little miracle growing inside you!